Employee Benefits at Work
Many Americans get health insurance at work. Once a year, employers have an "open enrollment" period when employees can make changes to their health insurance and other benefits for the coming year.
Choosing the right plan is important, and we're here to help you understand your options.
Determine Which Type of Plan is Best for You
Employers often provide several types of health insurance plans. The right plan for you will depend on factors such as your health care needs, budget, and preferred providers. See the most common types of health care plans offered by employers:
Health Maintenance Organization (HMO)
Cost: Usually has lower premiums and lower out-of-pocket costs.
Providers: Must use doctors within the plan's network, except in emergencies.
Primary Care Physician: You must have a primary care physician (PCP) who will manage your care and provide referrals to specialists.
Ideal for: Employees who are comfortable using a specific network of providers.
Preferred Provider Organization (PPO)
Cost: Typically has higher premiums and out-of-pocket costs than an HMO.
Providers: You can use any doctor, specialist, or hospital, with lower costs when choosing providers within the network.
Primary Care Physician: Not required, and you can see providers without a referral.
Ideal for: Employees who want freedom to choose health care providers.
Exclusive Provider Organization (EPO)
Cost: Typically has lower premiums and out-of-pocket costs than a PPO, but higher than an HMO.
Providers: Must stay within the plan’s network (except in emergencies). No coverage outside the network
Primary Care Physician: Typically not required, and specialist referrals are generally not needed.
Ideal for: Employees who want lower premiums but prefer not needing referrals.
High-Deductible Health Plan vs. Traditional Plan High-Deductible health plans require you to pay more health care costs yourself before the insurance company starts to pay its share. Traditional plans have lower deductibles, so the insurance company starts to pay its share more quickly in the year. There are often choices for both types with HMOs, PPOs, and EPOs.
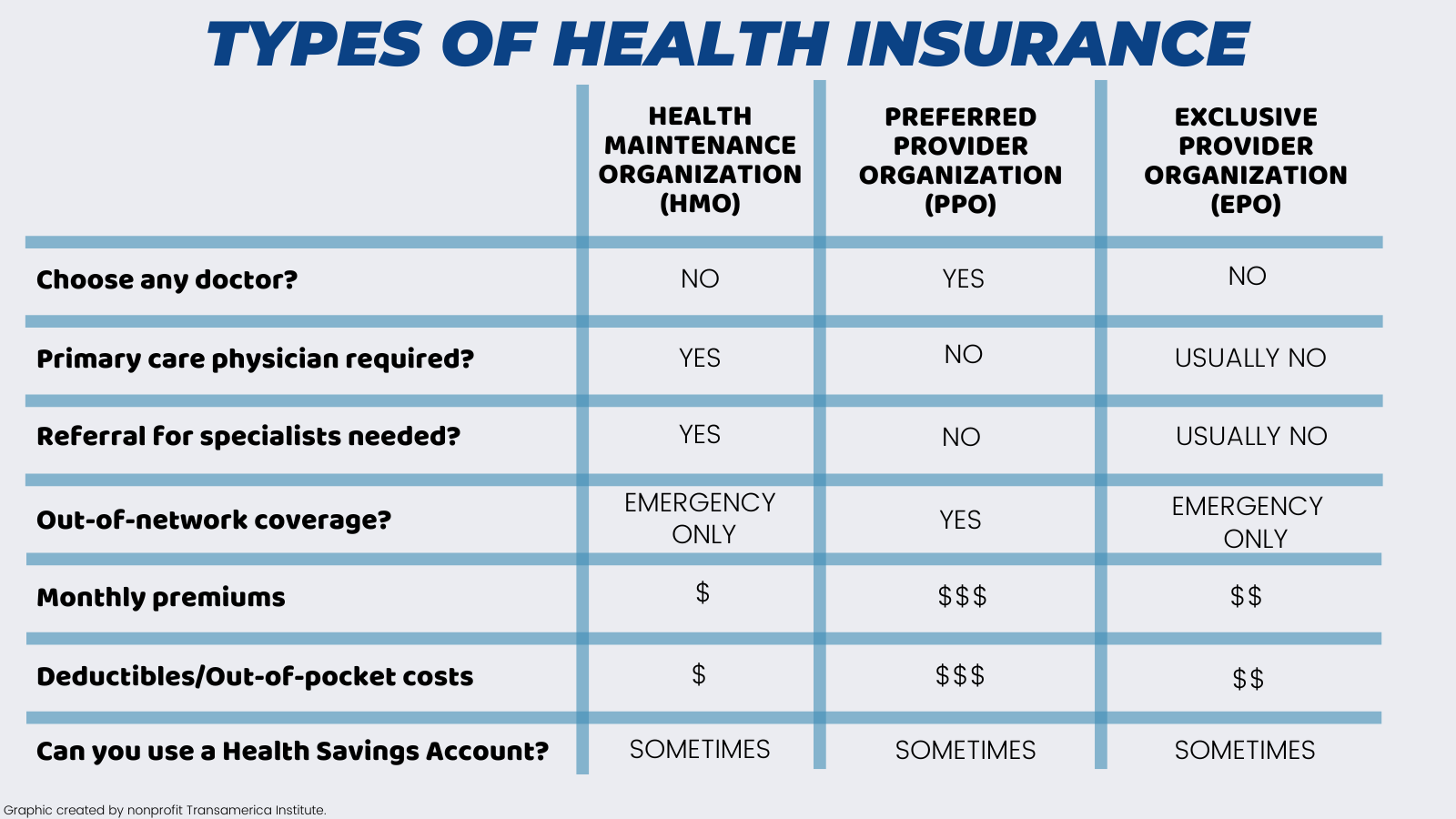
To compare these different plan types, consider the factors outlined in the chart below. Ask yourself which of these factors is most important to you, and then use the chart to determine which plan best fits your needs.
Understand Cost Components
Premium
The ongoing monthly payment that is deducted from your paycheck.
Deductible
The amount you pay before your health insurance starts to cover your bills. For example, if you have a $1,400 deductible, you must pay $1,400 out of pocket before your insurer starts covering the costs. Preventive care is typically paid by insurance even before your deductible is met.
Copay and Coinsurance
Plans vary. Some have a Copay which is a predetermined rate you pay for health care services at the time of care. For example, you may have a $40 copay every time you see your primary care physician. Other plans charge Coinsurance payments, where you pay a specified percentage of the service and the plan pays the rest, typically only after your deductible has been met. For example, if you have a 20% coinsurance, you pay 20% of each medical bill, and your health insurance pays 80%.
Compare Plan Costs, Benefits, and Provider Networks
Options for Managing Out-of-Pocket Costs
Health Savings Account (HSA)
A tax-advantaged medical savings account is available to those who are enrolled in a High-Deductible Health Plan. The funds contributed to the account aren’t subject to federal income tax at the time of deposit, the funds grow tax-deferred, and are not taxable when they are withdrawn to pay for qualified medical expenses at any point in your life. They are completely portable, meaning that if you change jobs, you keep the HSA account.
Health Care Flexible Spending Account (FSA)
A tax-advantaged medical savings account to pay for qualified health care costs, typically available to those who are not enrolled in a High-Deductible Health Plan. Like HSAs, the funds contributed to an FSA aren’t subject to federal income tax at the time of deposit, the funds grow tax-deferred, and are not taxable when they are withdrawn to pay for qualified medical expenses. However, you must use most of the funds in the year in which they were contributed (only a small portion can be rolled over to use the following year).
Check out Transamerica Institute's guide on HSA & FSA: What to Know to learn more.
Dependent Care Flexible Spending Account (FSA)
A tax-advantaged savings account to pay for eligible child and dependent elder care expenses you incur so you can work. Examples include preschool, after-school care for children up to age 13, adult day care, and in-home elder care. These funds must be used in the year they were contributed.
Health Reimbursement Arrangement (HRA)
An employer-funded account to pay for qualified health care costs. These are less common.
When to Enroll
When you start a new job
During your company's annual open enrollment
If you have a "qualifying" life event
Outside of the above enrollment periods, employees can only make changes to their coverage when they have a qualifying life event. Examples include getting married, having a baby, moving, losing health coverage through a spouse, or aging out of a parent's plan.
1936966 11/21